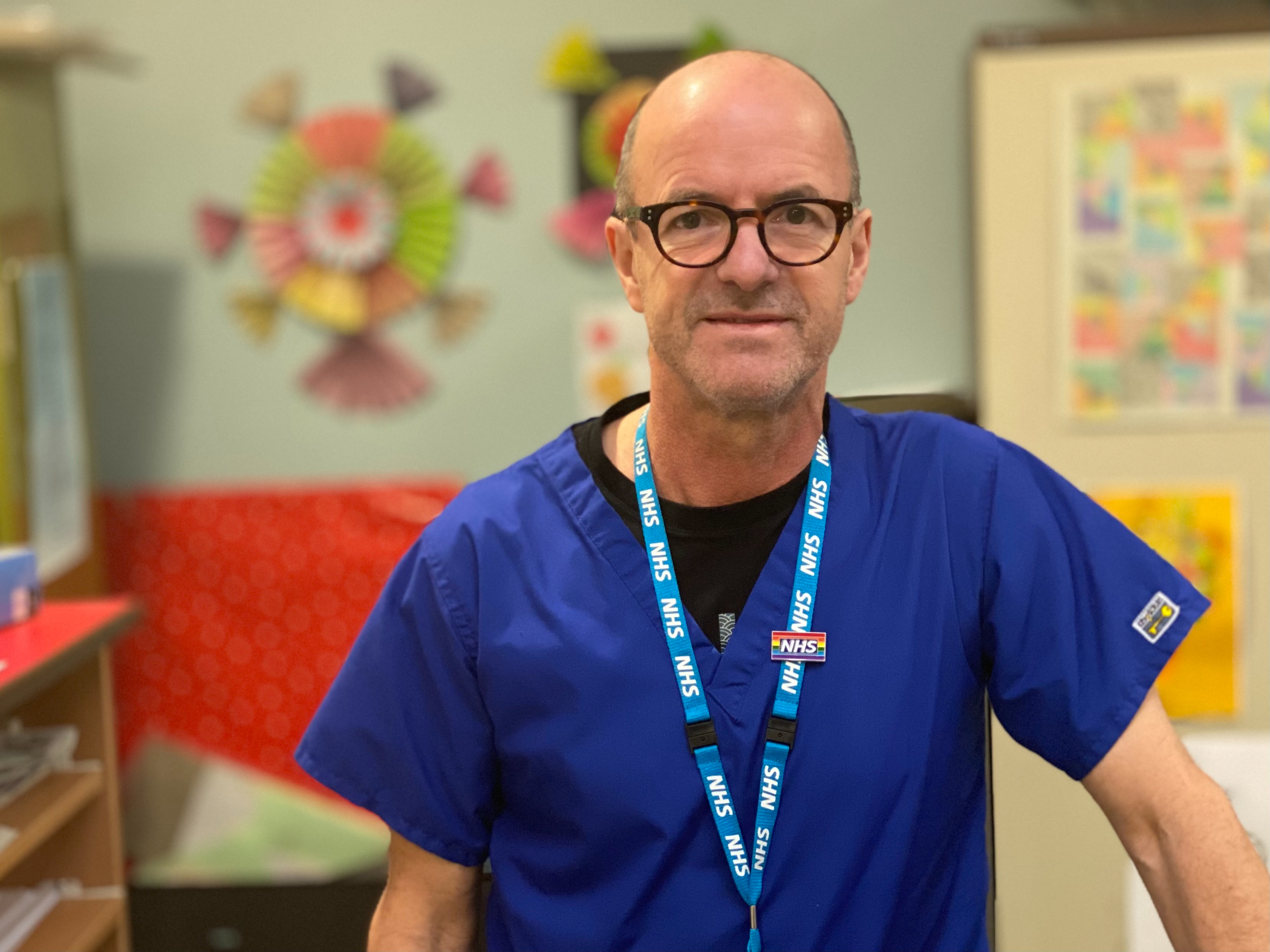
Adrian Jackson, a smoker of 40 years who works at RDaSH, has stopped smoking with QUIT.
“It’s never too late to quit. I was going to wait until my retirement but after speaking to the QUIT team, I decided to give it a go.
I used to smoke around 20 cigarettes a day. I didn’t see it as a problem but I did notice that I was getting out of breath a lot more. I did try to pack in a few years ago without success.
The difference this time is that I had the support round me which has really helped. It was a little tough especially after such a long time but I was determined to quit this time and I have."

A day in the life of...
Hayley Snowden | Health Improvement Manager | Sheffield Teaching Hospitals NHS Foundation Trust
My day usually starts around 830am. I get into the office and quickly catch up on what has happened over the previous day. Our Administration Officer pulls the referral report and I am given a list of patients to assess and follow up.
We are grouped into ward areas and today I’m covering the Respiratory wards. Here, I usually see patients who have COPD and have come into hospital with breathing difficulties. Their COPD Nurse will refer every smoker onto the QUIT Team so these can be our busiest wards.
My first patient is an lady who has asthma. As I arrive on the ward I introduce myself to the Staff Nurses and ask to be shown to the patient. I then complete my assessment, asking her questions about her smoking addiction and if she has tried to stop before.
Once the assessment is completed and treatment has been agreed I speak with her Nurse and ensure her medication is prescribed.
I then move on to my next patient who has been in hospital a while. I see him once a week to check he is doing OK, re-assess his NRT and chat about how he will remain smoke-free once he is at home.
Once I have visited all my patients, I move on to follow-up calls. Each patient who has been discharged from the hospital receives a phone call from our team to see how they are getting on at home.
The lady I call today is doing well. She received her treatment and is still smoke-free, but needs continued support to stay stopped by the Community Stop Smoking Service. Once I have finished on the phone to her I make the referral - the Community Team will continue to see her for up to 12 weeks.
At the end of the day I will check the hospital hot spots to remind them that the QUIT service is here to help in order to keep the hospital grounds smoke free!

QUIT will have a huge impact on so many people
“The implementation of the QUIT Programme across South Yorkshire and Bassetlaw hospitals will have a huge impact on the overall long-term health of so many people who smoke and will play a massive part in tackling smoking related health inequalities.
“I am very passionate about being part of this Programme and embedding it as routine practice within Barnsley Hospital, and supporting cultural change in how smoking is viewed as a disease that should be treated with medical intervention and not a lifestyle choice!
“All patients will have access specialist support during their hospital stay and hopefully see this as an opportunity to committing to quitting for good once they’re discharged.”
Laura Dixon, Health Improvement Manager (QUIT)
Barnsley Hospital NHS Foundation Trust
Understanding mental health care and tobacco addiction
Martin Lever, Health Improvement Manager at Sheffield Health and Social Care NHS Foundation Trust, shares his experiences advising mental health service users on the positive impact quitting smoking can have on their mental health.
There’s a common perception that smoking can help combat stress and anxiety, but in reality, that couldn’t be further from the truth.
When someone lights up a cigarette, they may get five minutes of relief from all their worries, but as soon as the withdrawal symptoms kick in shortly after the associated anxiety and irritability will have a far longer lasting, negative impact on their mental health.
This becomes especially problematic when you consider the smoking habits of individuals experiencing complex mental health issues, and it’s why our work delivering guidance through the QUIT programme to service users is so important.
Many people believe many mental health service users simply don’t want to quit smoking, because of their condition.
From the work we’ve done so far, I can say with confidence that this is a myth. The service users we’ve encountered in mental health settings are just as likely to be interested in quitting smoking as anyone else.
When people arrive with us on one of our mental health wards for the first time, they’re screened for their smoking status as part of routine procedure.
The value of the QUIT programme is it allows our specialist Tobacco Treatment Advisors to be patient, listen and build-up a relationship with service users at a point when their mental health could be at its worst.
Our aim isn’t to force people into quitting smoking, we just want to educate service users on the ways tobacco is affecting their physical and mental health.
You’d be surprised how many people don’t realise breathing any type of smoke is bad for their health, or that the conditions they suffer from – such as Chronic Obstructive Pulmonary Disease (COPD) – are likely a direct result of their smoking addiction.
We want to create a space for people to think about their tobacco dependence. I can personally empathise with anyone who finds the idea of quitting smoking incredibly daunting, because it took me four attempts to finally give up tobacco myself for good almost 14 years ago.
I know it’s not easy overcoming tobacco dependence, but the QUIT programme gives us the opportunity to discuss the benefits a smoke-free lifestyle offers with service users, and point them towards the support that’s freely available if they wish to take on the challenge.
Stop smoking programme will help Sonia see her grandson grow up
No smoker ever really believes their addiction will help land them in Accident & Emergency. But, that’s just what happened to Sonia Davis, 58, from Darton.
Sonia had been smoking for 50 years, incredibly having smoked her first cigarette when she was just eight years old. She said: “Kids my age used to think it was cool then to hang around with teenagers who smoked. They said to the younger kids ‘would you like to have a go at this’ and that was it.
“By the time I was 12 I was smoking in the house. We used to wait until Mum and Dad had gone to bed and then took all the roll-up dog ends apart to make new ones.”
When we spoke to Sonia in her hospital bed (June 18), it was a week after she she’d been rushed to Barnsley Hospital’s A&E. She explained: “It was a red-hot Sunday and we were having a family barbecue. I didn’t feel well and started having light sweats and couldn’t breathe.
“It felt like there were two vices around my chest. My partner was in the house and as soon as he saw what I was like he phoned an ambulance.”
Sonia’s blood pressure was sky high and she was admitted to hospital for tests and treatment. She said: “I had water on my lungs and the water was going to my legs and feet causing swelling. My breathing is affected and my kidneys are not filtering properly.
“Smoking has contributed; I had cut down to 10-15 cigs a day as I’d been feeling ‘phlegmy.’ But now if I get up just to go to the loo I have to lie down afterwards as I’m so out of breath.”
Sonia saw QUIT Programme Tobacco Treatment Advisors Leigh-Ann Saunderson and Moyra Ramsden, and is using nicotine patches and an inhalator to treat her tobacco addiction.
She is now back at home and said: “I still get breathless but not as bad. I still get the feeling that I want a cigarette but have resisted, my food tastes better. I’ve been smoke-free for three weeks.”
And Sonia has even more incentive to stay smoke-free – her new baby grandson Leo James. “I want to see him grow up,” she added.
![Sonia-Davis-2[2].jpg](/application/files/3216/2610/7609/Sonia-Davis-22.jpg)
No smoker ever really believes their addiction will help land them in Accident & Emergency. But, that’s just what happened to Sonia Davis, 58, from Darton.
Sonia has been smoking for 50 years, incredibly having smoked her first cigarette when she was just eight years old. She said: “Kids my age used to think it was cool then to hang around with teenagers who smoked. They said to the younger kids ‘would you like to have a go at this’ and that was it.
“By the time I was 12 I was smoking in the house. We used to wait until Mum and Dad had gone to bed and then took all the roll-up dog ends apart to make new ones.”
When we spoke to Sonia in her hospital bed (June 18), it was a week after she she’d been rushed to Barnsley Hospital’s A&E. She explained: “It was a red-hot Sunday and we were having a family barbecue. I didn’t feel well and started having light sweats and couldn’t breathe.
“It felt like there were two vices around my chest. My partner was in the house and as soon as he saw what I was like he phoned an ambulance.”
Sonia’s blood pressure was sky high and she was admitted to hospital for tests and treatment. She said: “I had water on my lungs and the water was going to my legs and feet causing swelling. My breathing is affected and my kidneys are not filtering properly.
“Smoking has contributed; I had cut down to 10-15 cigs a day as I’d been feeling ‘phlegmy.’ But now if I get up just to go to the loo I have to lie down afterwards as I’m so out of breath.”
Sonia saw QUIT Programme Tobacco Treatment Advisors Leigh-Ann Saunderson and Moyra Ramsden, and is using nicotine patches and an inhalator to treat her tobacco addiction.

She is now back at home and said: “I still get breathless but not as bad. I still get the feeling that I want a cigarette but have resisted, my food tastes better. I’ve been smoke-free for three weeks.”
And Sonia has even more incentive to stay smoke-free – her new baby grandson Leo James. “I want to see him grow up,” she added.
Sonia’s treatment is part of a ground-breaking stop smoking programme just launched across South Yorkshire and Bassetlaw. It has the potential to save up to 2,000 lives and 4,000 hospital readmissions a year.
The QUIT Programme is being delivered by South Yorkshire and Bassetlaw Integrated Care System (SYB ICS) in partnership with Yorkshire Cancer Research, five local authorities and local Stop Smoking Services.
Based on evidence from successful smaller schemes in Ottawa and in Greater Manchester, QUIT is the largest project of its kind in the world and will transform the way smoking is tackled by the NHS in the region.
Rather than seeing smoking as a lifestyle choice, hospital staff across eight NHS Trusts in South Yorkshire and Bassetlaw now recognise it as tobacco addiction – a medical condition they have a responsibility to treat as part of patients’ routine hospital care.
So, every hospital patient in the region over the age of 12 years who smokes will now have access to nicotine replacement treatments (NRT) and specialist stop smoking support during their hospital stay from 45 trained Tobacco Treatment Advisers funded by Yorkshire Cancer Research.
Dr Richard Jenkins, Chief Executive of Barnsley Hospital NHS Foundation Trust and Senior Responsible Officer for the QUIT Programme, said: “We know that smoking is the single greatest cause of preventable death, disability and illness so the QUIT initiative makes perfect sense – especially when it is our job as health professionals to reduce harm to health.
“By treating tobacco addiction, we will save lives, decrease inequalities in health and save the NHS money that can be reinvested in new services.”

![adrian jackson[2].jpg](/application/files/4916/1971/0038/adrian_jackson2.jpg)
